NHS Digital
NHS Data Model and Dictionary Service
| Type: | Patch |
| Reference: | 1586 |
| Version No: | 1.0 |
| Subject: | October 2016 Release Patch |
| Effective Date: | Immediate |
| Reason for Change: | Patch |
| Publication Date: | 26 October 2016 |
Background:
This patch updates the NHS Data Model and Dictionary in preparation for the October 2016 Release and includes:
- What's New amended to include Change Requests incorporated since the last version of the NHS Data Model and Dictionary was published.
- Missing hyperlinks added
- Website links updated
- HTML format corrected
- Retired Attribute links deleted from Classes
- Social Services Care Plan retired as it is not used in any data set.
To view a demonstration on "How to Read an NHS Data Model and Dictionary Change Request", visit the NHS Data Model and Dictionary help pages at: http://www.datadictionary.nhs.uk/Flash_Files/changerequest.htm.
Note: if the web page does not open, please copy the link and paste into the web browser.
Summary of changes:
| Date: | 26 October 2016 |
| Sponsor: | Richard Kavanagh, Head of Data Standards - Interoperability Specifications, Architecture, Standards and Innovation, NHS Digital |
Note: New text is shown with a blue background. Deleted text is crossed out. Retired text is shown in grey. Within the Diagrams deleted classes and relationships are red, changed items are blue and new items are green.
Click here for a printer friendly view of this page.
Change to Supporting Information: Changed Description
The purpose of the Automatic Identification and Data Capture for Patient Identification Data Set set is to support the accurate, timely and, therefore, safer identification of NHS PATIENTS in England, by encoding the key PATIENT identifiers into a GS1 DataMatrix 2D bar code which is printed on the identity band.The purpose of the Automatic Identification and Data Capture for Patient Identification Data Set set is to support the accurate, timely and, therefore, safer identification of NHS PATIENTS in England, by encoding the key PATIENT identifiers into a GS1 DataMatrix 2D bar code which is printed on the identity band. It is a technology enabling standard: implementation of this standard will enable subsequent processes involving the PATIENT and care provided to the PATIENT (where these processes are also bar coded) to be automatically identified using Automatic Identification and Data Capture (AIDC) techniques, e.g. bed management, phlebotomy, theatres management, medications administration and assets management.
The AIDC for Patient Identification Data Set provides an agreed national standard for printing in human readable forms of key PATIENT identifiers on the identity wristband, to support the accurate, timely and safer identification of NHS PATIENTS.
Change to Supporting Information: Changed Description
Introduction
The Neonatal Critical Care Minimum Data Set (NCCMDS) provides a record of what happens to a PATIENT when they receive Neonatal Critical Care in a Neonatal Intensive Care Unit, Maternity WARD, or Neonatal Transitional Care WARD.
The primary purpose of the Neonatal Critical Care Minimum Data Set is to allow the operation of the National Tariff Payment System within neonatal critical care. The Neonatal Critical Care Minimum Data Set supports the National Tariff Payment System by capturing the data needed to generate a Healthcare Resource Group (HRG) for each calendar day (or part thereof) of a period of neonatal critical care; these Healthcare Resource Groups are then used to inform the annual aggregate costing exercise, NHS Reference Costs.
Scope and Uses
The scope of the Neonatal Critical Care Minimum Data Set is:
a) All PATIENTS on a WARD with a CRITICAL CARE UNIT FUNCTION of National Code '13 - Neonatal Intensive Care Unit (Neonatal critical care patients predominate)'.
b) All PATIENTS (excluding Mothers) on a WARD with a CRITICAL CARE UNIT FUNCTION of National Code:
to whom one or more of the following CRITICAL CARE ACTIVITY CODES applies for a period greater than 4 hours:
| 01 | Respiratory support via a tracheal tube (Respiratory support via a tracheal tube provided) |
| 02 | Nasal Continuous Positive Airway Pressure (nCPAP) (PATIENT receiving nCPAP for any part of the day) |
| 04 | Exchange Transfusion (PATIENT received exchange transfusion) |
| 05 | Peritoneal Dialysis (PATIENT received Peritoneal Dialysis) |
| 06 | Continuous infusion of inotrope, pulmonary vasodilator or prostaglandin (PATIENT received a continuous infusion of an inotrope, vasodilator (includes pulmonary vasodilators) or prostaglandin) |
| 07 | Parenteral Nutrition (PATIENT receiving Parenteral Nutrition (amino acids +/- lipids)) |
| 08 | Convulsions (PATIENT having convulsions requiring treatment) |
| 09 | Oxygen Therapy (PATIENT receiving additional oxygen) |
| 10 | Neonatal abstinence syndrome (PATIENT receiving drug treatment for neonatal abstinence (withdrawal) syndrome) |
| 11 | Care of an intra-arterial catheter or chest drain (PATIENT receiving care of an intra-arterial catheter or chest drain) |
| 12 | Dilution Exchange Transfusion (PATIENT received Dilution Exchange Transfusion) |
| 13 | Tracheostomy cared for by nursing staff (PATIENT receiving care of tracheostomy cared for by nursing staff not by an external Carer (e.g. parent)) |
| 14 | Tracheostomy cared for by external Carer (PATIENT receiving care of tracheostomy cared for by an external Carer (e.g. parent) not by a NURSE) |
| 15 | Recurrent apnoea (PATIENT has recurrent apnoea needing frequent intervention, i.e. over 5 stimulations in 8 hours, or resuscitation with IPPV two or more times in 24 hours) |
| 16 | Haemofiltration (PATIENT received Haemofiltration) |
| 22 | Continuous monitoring (PATIENT requiring continuous monitoring (by mechanical monitoring equipment) of respiration or heart rate, or by transcutaneous transducers or by Saturation Monitors. Note: apnoea alarms and monitors are excluded as forms of continuous monitoring) |
| 23 | Intravenous glucose and electrolyte solutions (PATIENT being given intravenous glucose and electrolyte solutions) |
| 24 | Tube-fed (PATIENT being tube-fed) |
| 25 | Barrier nursed (PATIENT being barrier nursed) |
| 26 | Phototherapy (PATIENT receiving phototherapy) |
| 27 | Special monitoring (PATIENT receiving special monitoring of blood glucose or serum bilirubin measurement at a minimum frequency of more than one per calendar day) |
| 28 | Observations at regular intervals (PATIENT requiring recorded observations for temperature, heart rate, respiratory rate, blood pressure or scoring for neonatal abstinence syndrome. Recorded observations must be at a minimum frequency of 4 hourly) |
| 29 | Intravenous medication (PATIENT receiving intravenous medication) |
| 80 | Heated Humidified High Flow Therapy (HHHFT) (PATIENT receiving HHHFT) |
| 81 | Presence of an umbilical venous line |
| 82 | Continuous infusion of insulin (PATIENT receiving a continuous infusion of insulin) |
| 83 | Therapeutic hypothermia (PATIENT receiving therapeutic hypothermia) |
| 84 | PATIENT has a Replogle tube in situ |
| 85 | PATIENT has an epidural catheter in situ |
| 86 | PATIENT has an abdominal silo |
| 87 | Administration of intravenous (IV) blood products |
| 88 | PATIENT has a central venous or long line (Peripherally Inserted Central Catheter line) in situ |
| 89 | PATIENT has an indwelling urinary or suprapubic catheter in situ |
| 90 | PATIENT has a trans-anastomotic tube in situ following oesophageal atresia repair |
| 91 | PATIENT has confirmed clinical seizure(s) today and/or continuous cerebral function monitoring (CFM) |
| 92 | PATIENT has a ventricular tap via needle or reservoir today |
| 93 | PATIENT has a stoma |
This data is captured and recorded locally and may be used for the purposes of direct care, clinical audit, Reference Costs, and other local uses. Any transmission of the Neonatal Critical Care Minimum Data Set must be covered by fair processing arrangements in accordance with information governance criteria and appropriate local arrangements.
Commissioning Data Set Transmission
Subject to the Commissioning Data Set Version 6-2 XML Schema Constraints, the Neonatal Critical Care Minimum Data Set is carried into the Secondary Uses Service (SUS) as a part of the following Commissioning Data Set messages, see SCCI0075:
Subject to the Commissioning Data Set Version 6-2 XML Schema Constraints, the Neonatal Critical Care Minimum Data Set is carried into the Secondary Uses Service (SUS) as a part of the following Commissioning Data Set messages, see SCCI0075:
- CDS V6-2 Type 130 - Admitted Patient Care - Finished General Episode Commissioning Data Set
- CDS V6-2 Type 180 - Admitted Patient Care - Unfinished Birth Episode Commissioning Data Set
- CDS V6-2 Type 190 - Admitted Patient Care - Unfinished General Episode Commissioning Data Set
The Secondary Uses Service groups this data into neonatal critical care Healthcare Resource Groups; these are a mandated currency under the National Tariff Payment System. Further guidance can be found on the NHS Digital website at: SCCI0075. Further guidance can be found on the NHS Digital website at: SCCI0075.
Change to Supporting Information: Changed Description
The NHS Data Model and Dictionary Service is provided by NHS Digital.
The NHS Data Model and Dictionary Service provides the development, maintenance and support of NHS Information Standards, contained in the NHS Data Model and Dictionary.
The NHS Data Model and Dictionary Service provides the following products and information to help users understand and navigate the NHS Data Model and Dictionary:
- Mailing List
- Submitting A Query
- Help Pages
- Frequently Asked Questions
- Policy and Supporting Documents etc.
For further information on the NHS Data Model and Dictionary Service, see the NHS Data Model and Dictionary Service web pages on the NHS Digital website.
Change to Supporting Information: Changed Description
Introduction
The Paediatric Critical Care Minimum Data Set (PCCMDS) provides a record of what happens to a PATIENT when they receive Paediatric Critical Care in a Paediatric Intensive Care Unit, or other critical care setting suitable for children.
The primary purpose of the Paediatric Critical Care Minimum Data Set is to allow the operation of the National Tariff Payment System within paediatric critical care. The Paediatric Critical Care Minimum Data Set supports the National Tariff Payment System by capturing the data needed to generate a Healthcare Resource Group (HRG) for each calendar day (or part thereof) of a period of paediatric critical care; these Healthcare Resource Groups are then used to inform the annual aggregate costing exercise, NHS Reference Costs.
Scope and Uses
The scope of the Paediatric Critical Care Minimum Data Set is:
a) All PATIENTS on a WARD with a CRITICAL CARE UNIT FUNCTION of National Code '04 - Paediatric Intensive Care Unit (Paediatric critical care patients predominate)'
b) All PATIENTS on a WARD with a CRITICAL CARE UNIT FUNCTION of National Code of either:
- 16 - Ward for children and young people
- 17 - High Dependency Unit for children and young people
- 18 - Renal Unit for children and young people
- 19 - Burns Unit for children and young people
- 92 - Non standard location using the operating department for children and young people
to whom one or more of the following CRITICAL CARE ACTIVITY CODES applies for a period greater than 4 hours:
| 04 | Exchange Transfusion (PATIENT received exchange transfusion) |
| 05 | Peritoneal dialysis (acute PATIENTS only i.e. excluding chronic) * |
| 06 | Continuous infusion of inotrope, pulmonary vasodilator or prostaglandin (PATIENT received a continuous infusion of an inotrope, vasodilator (includes pulmonary vasodilators) or prostaglandin) |
| 09 | Oxygen Therapy (supplementary Oxygen Therapy, irrespective of ventilatory state) ** |
| 13 | Tracheostomy cared for by nursing staff (PATIENT receiving care of tracheostomy cared for by nursing staff not by an external Carer (e.g. parent)) |
| 16 | Haemofiltration (PATIENT received Haemofiltration) |
| 50 | Continuous electrocardiogram monitoring |
| 51 | Invasive ventilation via endotracheal tube |
| 52 | Invasive ventilation via tracheostomy tube |
| 53 | Non-invasive ventilatory support |
| 55 | Nasopharyngeal airway |
| 56 | Advanced ventilatory support (Jet or Oscillatory ventilation) |
| 57 | Upper airway obstruction requiring nebulised Epinephrine/ Adrenaline |
| 58 | Apnoea requiring intervention |
| 59 | Acute severe asthma requiring intravenous bronchodilator therapy or continuous nebuliser |
| 60 | Arterial line monitoring |
| 61 | Cardiac pacing via an external box (pacing wires or external pads or oesophageal pacing) |
| 62 | Central venous pressure monitoring |
| 63 | Bolus intravenous fluids (> 80 ml/kg/day) in addition to maintenance intravenous fluids |
| 64 | Cardio-pulmonary resuscitation (CPR) |
| 65 | Extracorporeal membrane oxygenation (ECMO) or Ventricular Assist Device (VAD) or aortic balloon pump |
| 66 | Haemodialysis (acute PATIENTS only i.e. excluding chronic) |
| 67 | Plasma filtration or Plasma exchange |
| 68 | ICP-intracranial pressure monitoring |
| 69 | Intraventricular catheter or external ventricular drain |
| 70 | Diabetic ketoacidosis (DKA) requiring continuous infusion of insulin |
| 71 | Intravenous infusion of thrombolytic agent (limited to tissue plasminogen activator [tPA] and streptokinase) |
| 72 | Extracorporeal liver support using Molecular Absorbent Liver Recirculating System (MARS) |
| 73 | Continuous pulse oximetry |
| 74 | PATIENT nursed in single occupancy cubicle |
| 80 | Heated Humidified High Flow Therapy (HHHFT) (PATIENT receiving HHHFT) |
| 85 | PATIENT has an epidural catheter in situ |
| 94 | PATIENT has arrhythmia requiring intravenous anti-arrhythmic therapy |
| 95 | PATIENT has reduced conscious level (Glasgow Coma Score 12 or below) and hourly (or more frequent) Glasgow Coma Score monitoring |
| 96 | Intravenous infusion of sedative agent (PATIENT receiving continuous intravenous infusion of sedative agent) |
| 97 | PATIENT has status epilepticus requiring treatment with continuous intravenous infusion |
Notes:
- ** National Code 09 applies as an inclusion criterion when the PATIENT receives supplementary Oxygen Therapy, irrespective of their ventilatory state.
This data is captured and recorded locally and may be used for the purposes of direct care, clinical audit, Reference Costs, and other local uses. Any transmission of the Paediatric Critical Care Minimum Data Set must be covered by fair processing arrangements in accordance with information governance criteria and appropriate local arrangements.
Commissioning Data Set Transmission
Subject to the Commissioning Data Set Version 6-2 XML Schema Constraints, the Paediatric Critical Care Minimum Data Set is sent to the Secondary Uses Service (SUS) as a part of the following Commissioning Data Set messages, SCCI0076:Subject to the Commissioning Data Set Version 6-2 XML Schema Constraints, the Paediatric Critical Care Minimum Data Set is sent to the Secondary Uses Service (SUS) as a part of the following Commissioning Data Set messages, SCCI0076:
The Secondary Uses Service groups this data into paediatric critical care Healthcare Resource Groups. Further guidance can be found on the NHS Digital website at: SCCI0076. Further guidance can be found on the NHS Digital website at: SCCI0076.
Change to Supporting Information: Changed status to Retired, Name, Description
A Social Services Care Plan is a CARE PLAN.This item has been retired from the NHS Data Model and Dictionary.
A Social Services Care Plan is a CARE PLAN which identifies the type of social services care a Child or Young Person is receiving.The last live version of this item is available in the September 2016 release of the NHS Data Model and Dictionary.
Change to Supporting Information: Changed status to Retired, Name, Description
- Retired Social Services Care Plan
- Changed Name from Data_Dictionary.NHS_Business_Definitions.S.Social_Services_Care_Plan to Retired.Data_Dictionary.NHS_Business_Definitions.S.Social_Services_Care_Plan
- Changed Description
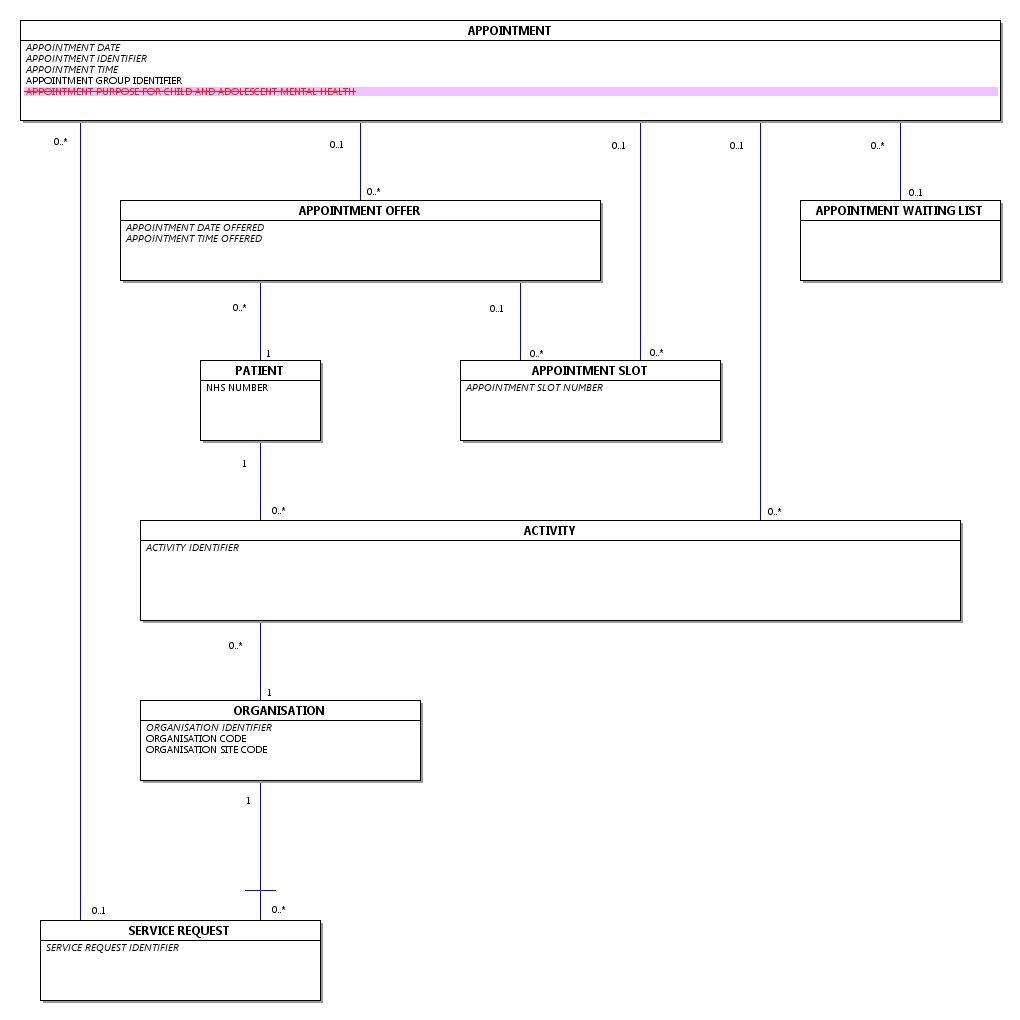
Change to Class: Changed Attributes
| K | APPOINTMENT DATE | |
| K | APPOINTMENT IDENTIFIER | |
| K | APPOINTMENT TIME | |
| APPOINTMENT CANCELLED DATE | ||
| APPOINTMENT FIRST ATTENDANCE | ||
| APPOINTMENT GROUP IDENTIFIER | ||
| APPOINTMENT TYPE | ||
| APPOINTMENT TYPE FOR IMPROVING ACCESS TO PSYCHOLOGICAL THERAPIES | ||
| ATTENDED OR DID NOT ATTEND | ||
| DID NOT ATTEND REASON | ||
| INVITATION OFFER SENT INDICATOR | ||
| UNIQUE BOOKING REFERENCE NUMBER CONVERTED |
Change to Attribute: Changed Description
The type of CARE PLAN.
National Codes:
| 01 | Cancer Care Plan |
| 02 | Child Protection Plan |
| 03 | Mental Health Crisis Plan |
| 04 | Social Services Care Plan (Retired 01 September 2015) |
| 05 | Antenatal Care Plan |
| 06 | Birth Care Plan |
| 07 | Postpartum Care Plan |
| 08 | Education, Health and Care Plan (EHC) |
Change to Attribute: Changed Description
National Codes:
| 01 | Respiratory support via a tracheal tube (Respiratory support via a tracheal tube provided) |
| 02 | Nasal Continuous Positive Airway Pressure (nCPAP) (PATIENT receiving nCPAP for any part of the day) |
| 03 | Surgery (PATIENT received surgery) |
| 04 | Exchange Transfusion (PATIENT received exchange transfusion) |
| 05 | Peritoneal Dialysis (PATIENT received Peritoneal Dialysis) |
| 06 | Continuous infusion of inotrope, pulmonary vasodilator or prostaglandin (PATIENT received a continuous infusion of an inotrope, vasodilator (includes pulmonary vasodilators) or prostaglandin) |
| 07 | Parenteral Nutrition (PATIENT receiving Parenteral Nutrition (amino acids +/- lipids)) |
| 08 | Convulsions (PATIENT having convulsions requiring treatment) |
| 09 | Oxygen Therapy (PATIENT receiving additional oxygen) |
| 10 | Neonatal abstinence syndrome (PATIENT receiving drug treatment for neonatal abstinence (withdrawal) syndrome) |
| 11 | Care of an intra-arterial catheter or chest drain (PATIENT receiving care of an intra-arterial catheter or chest drain) |
| 12 | Dilution Exchange Transfusion (PATIENT received Dilution Exchange Transfusion) |
| 13 | Tracheostomy cared for by nursing staff (PATIENT receiving care of tracheostomy cared for by nursing staff not by an external Carer (e.g. parent)) |
| 14 | Tracheostomy cared for by external Carer (PATIENT receiving care of tracheostomy cared for by an external Carer (e.g. parent) not by a NURSE) |
| 15 | Recurrent apnoea (PATIENT has recurrent apnoea needing frequent intervention, i.e. over 5 stimulations in 8 hours, or resuscitation with IPPV two or more times in 24 hours) |
| 16 | Haemofiltration (PATIENT received Haemofiltration) |
| 21 | Carer Resident - Caring for Baby (External Carer (for example, parent) resident with the baby and reducing nursing required by caring for the baby) |
| 22 | Continuous monitoring (PATIENT requiring continuous monitoring (by mechanical monitoring equipment) of respiration or heart rate, or by transcutaneous transducers or by Saturation Monitors. Note: apnoea alarms and monitors are excluded as forms of continuous monitoring) |
| 23 | Intravenous glucose and electrolyte solutions (PATIENT being given intravenous glucose and electrolyte solutions) |
| 24 | Tube-fed (PATIENT being tube-fed) |
| 25 | Barrier nursed (PATIENT being barrier nursed) |
| 26 | Phototherapy (PATIENT receiving phototherapy) |
| 27 | Special monitoring (PATIENT receiving special monitoring of blood glucose or serum bilirubin measurement at a minimum frequency of more than one per calendar day) |
| 28 | Observations at regular intervals (PATIENT requiring recorded observations for temperature, heart rate, respiratory rate, blood pressure or scoring for neonatal abstinence syndrome. Recorded observations must be at a minimum frequency of 4 hourly) |
| 29 | Intravenous medication (PATIENT receiving intravenous medication) |
| 50 | Continuous electrocardiogram monitoring |
| 51 | Invasive ventilation via endotracheal tube |
| 52 | Invasive ventilation via tracheostomy tube |
| 53 | Non-invasive ventilatory support |
| 55 | Nasopharyngeal airway |
| 56 | Advanced ventilatory support (Jet or Oscillatory ventilation) |
| 57 | Upper airway obstruction requiring nebulised Epinephrine/ Adrenaline |
| 58 | Apnoea requiring intervention |
| 59 | Acute severe asthma requiring intravenous bronchodilator therapy or continuous nebuliser |
| 60 | Arterial line monitoring |
| 61 | Cardiac pacing via an external box (pacing wires or external pads or oesophageal pacing) |
| 62 | Central venous pressure monitoring |
| 63 | Bolus intravenous fluids (> 80 ml/kg/day) in addition to maintenance intravenous fluids |
| 64 | Cardio-pulmonary resuscitation (CPR) |
| 65 | Extracorporeal membrane oxygenation (ECMO) or Ventricular Assist Device (VAD) or aortic balloon pump |
| 66 | Haemodialysis (acute PATIENTS only i.e. excluding chronic) |
| 67 | Plasma filtration or Plasma exchange |
| 68 | ICP-intracranial pressure monitoring |
| 69 | Intraventricular catheter or external ventricular drain |
| 70 | Diabetic ketoacidosis (DKA) requiring continuous infusion of insulin |
| 71 | Intravenous infusion of thrombolytic agent (limited to tissue plasminogen activator [tPA] and streptokinase) |
| 72 | Extracorporeal liver support using Molecular Absorbent Liver Recirculating System (MARS) |
| 73 | Continuous pulse oximetry |
| 74 | PATIENT nursed in single occupancy cubicle |
| 80 | Heated Humidified High Flow Therapy (HHHFT) (PATIENT receiving HHHFT) * |
| 81 | Presence of an umbilical venous line * |
| 82 | Continuous infusion of insulin (PATIENT receiving a continuous infusion of insulin) * |
| 83 | Therapeutic hypothermia (PATIENT receiving therapeutic hypothermia) * |
| 84 | PATIENT has a Replogle tube in situ * |
| 85 | PATIENT has an epidural catheter in situ * |
| 86 | PATIENT has an abdominal silo * |
| 87 | Administration of intravenous (IV) blood products * |
| 88 | PATIENT has a central venous or long line (Peripherally Inserted Central Catheter line) in situ * |
| 89 | PATIENT has an indwelling urinary or suprapubic catheter in situ * |
| 90 | PATIENT has a trans-anastomotic tube in situ following oesophageal atresia repair * |
| 91 | PATIENT has confirmed clinical seizure(s) today and/or continuous cerebral function monitoring (CFM) * |
| 92 | PATIENT has a ventricular tap via needle or reservoir today * |
| 93 | PATIENT has a stoma * |
| 94 | PATIENT has arrhythmia requiring intravenous anti-arrhythmic therapy * |
| 95 | PATIENT has reduced conscious level (Glasgow Coma Score 12 or below) and hourly (or more frequent) Glasgow Coma Score monitoring * |
| 96 | Intravenous infusion of sedative agent (PATIENT receiving continuous intravenous infusion of sedative agent) * |
| 97 | PATIENT has status epilepticus requiring treatment with continuous intravenous infusion * |
| 99 | No Defined Critical Care Activity (PATIENT is not receiving any of the critical care interventions listed above (Excluding code 21). For example, PATIENT is on the Intensive Care Unit ready for discharge and is receiving normal care. This is the default code. |
* Note - National Codes 80-97 should not be reported nationally until the functionality to do so becomes available in the next release of the Commissioning Data Sets and the associated XML Schema. Prior to this release, these codes must be recorded locally, however the National Codes 80-97 cannot be transmitted in the current version of the Commissioning Data Sets (Version 6-2). Further guidance can be found on the NHS Digital website at: SCCI0075 and SCCI0076. Further guidance can be found on the NHS Digital website at: SCCI0075 and SCCI0076.
Change to Data Element: Changed Description
This item has been retired from the NHS Data Model and Dictionary.
The last live version of this item is available in the August 2016 release of the NHS Data Model and Dictionary.
Access to this version can be obtained by emailing information.standards@hscic.gov.uk with "NHS Data Model and Dictionary - Archive Request" in the email subject line.Access to this version can be obtained by emailing information.standards@nhs.net with "NHS Data Model and Dictionary - Archive Request" in the email subject line.
Change to Data Element: Changed Description
| Format/Length: | min an5 max an9 |
| National Codes: | |
| ODS Default Codes: | 89999 - Non-NHS UK Provider where no ORGANISATION IDENTIFIER has been issued |
| 89997 - Non-UK Provider where no ORGANISATION IDENTIFIER has been issued |
Notes:
ORGANISATION SITE IDENTIFIER (OF IMAGING) is the same as attribute ORGANISATION IDENTIFIER.
ORGANISATION SITE IDENTIFIER (OF IMAGING) is the ORGANISATION IDENTIFIER where the Diagnostic Imaging took place.ORGANISATION SITE IDENTIFIER (OF IMAGING) is the ORGANISATION IDENTIFIER of the Organisation Site where the Diagnostic Imaging took place.
SITE CODE (OF IMAGING) will be replaced with ORGANISATION SITE IDENTIFIER (OF IMAGING), when it has been approved for use in national information standards.
For enquiries about this Change Request, please email information.standards@nhs.net